How antibiotics works? 💊
By: HWC
Date Uploaded: 04/11/2020
Tags: homeworkclinic.com Homework Clinic HWC antibiotic resistance Alexander Fleming penicillin harmful bacteria Tetracycline natural selection plasmid
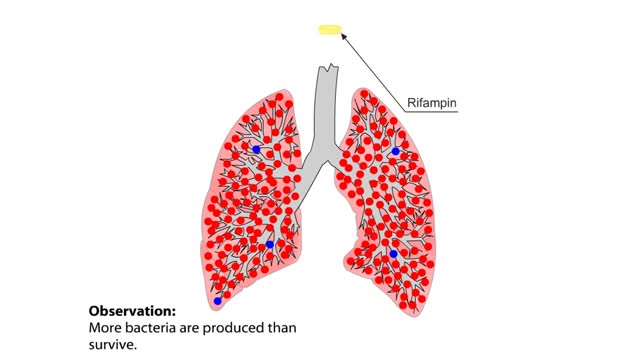
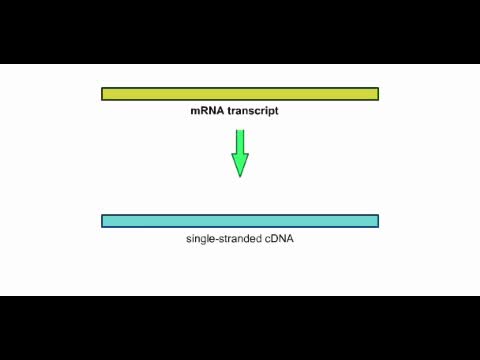
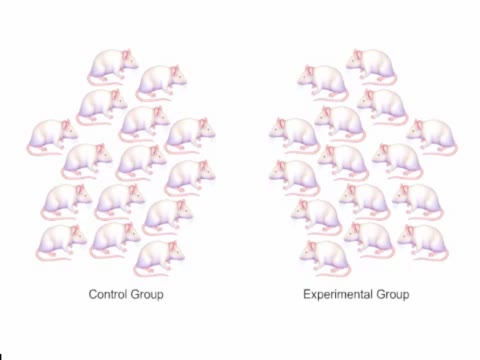
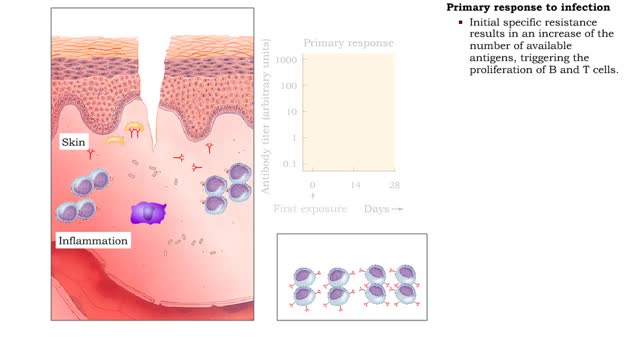
The Crisis in Antibiotic Resistance More than 70 years ago, Alexander Fleming discovered penicillin. A few decades later, when this antibiotic was used in World War II, Fleming's discovery had revolutionized medicine. No longer did people have to die from something as trivial as an infected cut.Yet, even as we enjoy the benefits of antibiotics, their use promotes antibiotic resistance in bacteria. By confronting bacteria with antibiotics, we select for those that are resistant and change the course of their evolution. One reason that many bacteria become more resistant is that antibiotics are often used inappropriately. Many doctors prescribe antibiotics for the common cold, even though most colds are caused by viruses, which antibiotics can do nothing to halt. Also, the agricultural practice in many countries is to add antibiotics to animal feed to promote growth. If we don't educate each other on the prudent use of antibiotics, we will continue to race toward a crisis in antibiotic resistance. Bacteria are becoming resistant to many of the antibiotics in our medical arsenal. One reason for the widespread resistance lies in the indiscriminant use of antibiotics. For example, at the insistence of patients, doctors often prescribe antibiotics even for the common cold. Antibiotics have no effect on viruses, and viruses cause most colds. Antibiotics attack bacteria. There are millions of bacteria in the body. Most are found in the gut and are either harmless or beneficial. Some of these bacteria are beneficial because they make vitamins that the body can use. Also, by competing for space and nutrients, the many species of bacteria prevent each other, as well as harmful bacteria, from multiplying out of control. What happens to the resident bacteria when a person takes antibiotics? If the person has never taken this particular antibiotic before, then most of the bacteria would probably be susceptible to it. Antibiotics work by a variety of mechanisms. Tetracycline, for example, binds to ribosomes in bacteria and jams the production of proteins. From lack of protein production, a bacterium dies. Most of the bacteria die, but, by chance, a few may have mutations that allow them to live in the presence of the antibiotic. Their mutations might cause their ribosomes to have a slightly different structure, which prevents the antibiotic from binding. With these mutations, the bacteria can still make proteins and survive in the presence of the antibiotic. They are resistant. The antibiotic treatment provides an example of natural selection in action. In the presence of antibiotics, susceptible bacteria die, but resistant bacteria have an advantage and multiply. The bacteria reproduce asexually and therefore make identical copies of the original cells. The populations of bacteria evolve, with the proportion of resistant bacteria greatly increased. Once established, resistance is hard to eliminate, and the resistance may spread to different species of bacteria. The easiest way of spreading resistance is when the resistance gene is located on a loop of DNA called a plasmid. We've already seen how resistance can occur when the antibiotic's target, such as the ribosome, changes. However other antibiotics work by different mechanisms. In another type of resistance, a gene might code for a transport protein that pumps antibiotics out of the bacterial cell, preventing the antibiotics from harming the bacterium. In another type of resistance, a gene might code for an enzyme that breaks apart antibiotic molecules. The ability to resist an antibiotic can be gained by plasmid transfer. In a frightening, yet realistic, scenario a relatively harmless bacterium transfers its resistance genes to a highly pathogenic species.
Add To
You must login to add videos to your playlists.
Advertisement



Comments
0 Comments total
Sign In to post comments.
No comments have been posted for this video yet.